

Positive serology (rheumatoid factor and anti-citrullinated protein antibody), as well as elevated inflammatory markers, may help confirm the diagnosis. The updated classification criteria for RA from the American College of Rheumatology ( Table 1 6) no longer include the presence of rheumatoid nodules or radiographic erosive changes, both of which are less likely in early presentation. Radiography may be helpful in differentiation if the typical periarticular erosions of RA are present. Physicians must use history and physical examination findings to differentiate the inflammatory arthritis in RA from another etiology, including systemic lupus erythematosus, systemic sclerosis, psoriatic arthritis, sarcoidosis, crystal arthropathy, and spondyloarthropathy. Diagnosis and management of rheumatoid arthritis. Reprinted with permission from Wasserman AM.
#RHEUMATOID ARTHRITIS DIAGNOSIS CRITERIA 2020 SKIN#
Note that the skin creases over the proximal interphalangeal joints become less apparent with swelling. Boggy swelling caused by synovitis may be visible ( Figure 1 5), or subtle synovial thickening may be palpable on joint examination.īoggy swelling in proximal interphalangeal and metacarpophalangeal joints (more prominent on patient's right hand) in a patient with new-onset rheumatoid arthritis. Patients may also present with systemic symptoms of fatigue, weight loss, and anemia. Morning stiffness lasting more than one hour suggests an inflammatory etiology. The distal interphalanges and lumbar spine are not typically impacted by RA. RA typically presents with pain and stiffness in multiple joints, most often the wrists, proximal interphalangeal joints, and metacarpophalangeal joints. Women, smokers, and those with a family history of the disease are at higher risk. RA onset can occur at any age, but it peaks between 30 and 50 years of age.
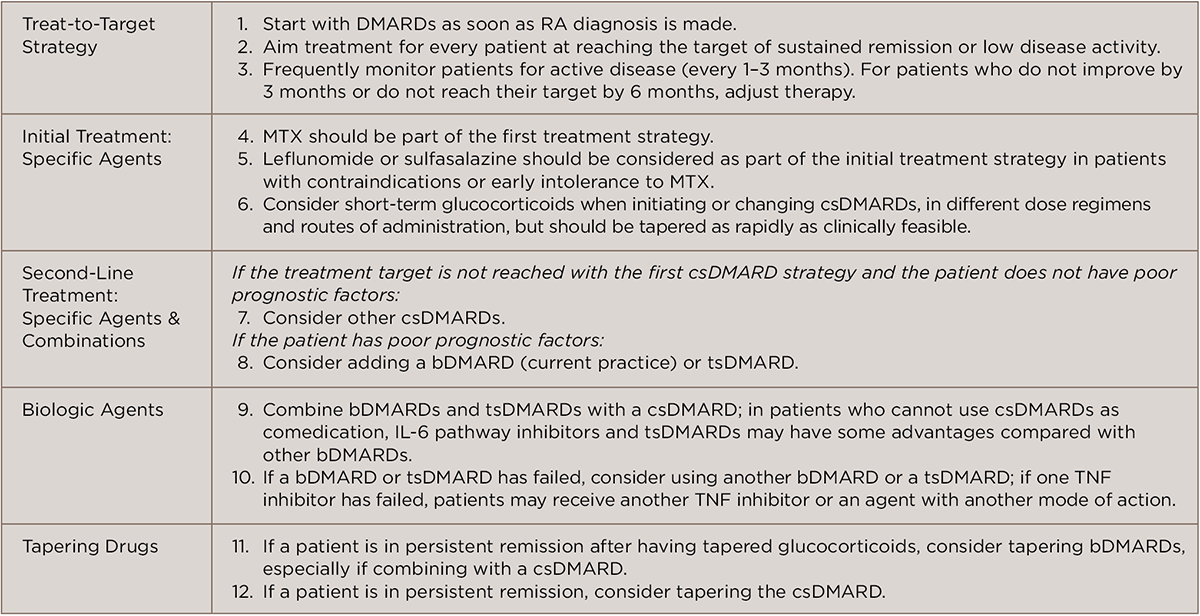
Rheumatoid arthritis (RA) is the most common autoimmune inflammatory arthritis, with a lifetime prevalence of up to 1% worldwide. Although rheumatoid arthritis is often a chronic disease, some patients can taper and discontinue medications and remain in long-term remission. Comorbid conditions, including hepatitis B or C or tuberculosis infections, must be considered when choosing medical treatments. Additional disease-modifying antirheumatic drugs or biologic agents should be added if disease activity persists. Methotrexate is typically the first-line agent for rheumatoid arthritis. The goal of therapy is to initiate early medical treatment to achieve disease remission or the lowest disease activity possible. Rapid diagnosis of rheumatoid arthritis allows for earlier treatment with disease-modifying antirheumatic drugs, which is associated with better outcomes. Rheumatoid arthritis may impact organs other than the joints, including lungs, skin, and eyes. In a patient with inflammatory arthritis, the presence of a rheumatoid factor and/or anti-citrullinated protein antibody, elevated C-reactive protein level, or elevated erythrocyte sedimentation rate is consistent with a diagnosis of rheumatoid arthritis. Rheumatoid arthritis should be considered if there is at least one joint with definite swelling that is not better explained by another disease. Women, smokers, and those with a family history of the disease are most often affected. Rheumatoid arthritis is the most commonly diagnosed systemic inflammatory arthritis, with a lifetime prevalence of up to 1% worldwide.


 0 kommentar(er)
0 kommentar(er)
